Abstract
Background: Intracranial hemorrhage (ICH) frequently complicates the clinical course of patients with brain tumors. These bleeding events carry significant morbidity and portend poor survival outcomes. The frequent need to prescribe antiplatelet medications, including aspirin and P2Y12 inhibitors, further complicates the risk of hemorrhage in this patient population with concurrent cardiovascular or cerebrovascular indications. The impact of these agents on rates of ICH in the general population has previously been studied and remains equivocal. Whether antiplatelet medications increase the risk of ICH in primary brain tumors remains undefined, and there is limited evidence to guide their use in this setting.
Aims: We investigated whether patients with primary brain tumors receiving antiplatelet medications had an increased risk of ICH compared to a matched cohort.
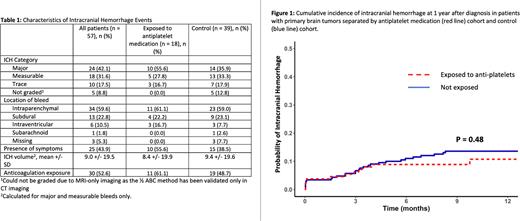
Methods: This study was a retrospective matched cohort study of patients with diagnosis of primary brain tumor treated at our center between 2010-2021. Patients with metastatic brain disease were excluded. Patients treated with antiplatelet medications (aspirin and P2Y12 inhibitors) were matched with patients not receiving these agents. Matching was performed using a scoring algorithm that ranked controls according to cancer type, exposure to anticoagulation, age, sex, and year of diagnosis. The primary end point of the study was the cumulative incidence of ICH at 1 year after tumor diagnosis. Radiologic images of bleeding events were assessed by a neuroradiologist blinded to the study cohort allocation. ICH was defined as trace (< 1 cm3), measurable (1 - 10 cm3), or major (symptomatic or > 10 cm3), with bleed volumes defined by the ½ ABC method.
Results: The study population included 398 patients with primary brain tumors. 134 patients were exposed to antiplatelet medications. Of these 134 patients, 123 were exposed to aspirin alone, 10 were exposed to dual antiplatelet therapy (aspirin and P2Y12 inhibitor), and 1 received P2Y12 inhibitor alone. The most common malignancy in the study cohort was glioma (78%). The cumulative incidence of ICH at 1 year was 10.8% (95% CI, 5.2 - 16.3) in those receiving antiplatelet agents compared with 13.6% (95% CI, 9.0 - 18.2) in the control population (P = 0.48, Gray test). The cumulative incidence of major ICH at 1 year was 7.2% (95% CI, 2.6 - 11.7) in those receiving antiplatelet agents compared to 4.8% (95% CI, 2.0 - 7.5) among controls (P = 0.48, Gray test) (Figure 1). The distribution of ICH volume size was similar in the 2 groups (Table 1). The combined use of antiplatelet medication with anticoagulation did not increase the risk of total ICH compared to patients that did not receive either (HR 1.53, 95% CI 0.74 - 3.17) but did increase the risk of major ICH compared with patients that did not receive either (HR 3.41, 95% CI 1.04 - 11.19, P = 0.043). Median overall survival in patients exposed to antiplatelet medications was 28.3 months (95% CI, 19.6 - 47.9) compared to 20.8 months in those not exposed (95% CI, 16.6 - 30.6, P = 0.09).
Conclusions: In patients with primary brain tumors, administration of antiplatelet medications was not associated with an increased incidence of ICH. However, there was an increased risk of major ICH for patients exposed to both antiplatelet medication and anticoagulation.
Disclosures
Neuberg:Madrigal Pharmaceuticals: Current equity holder in private company. Zwicker:Pfizer/BMS: Honoraria; Portola: Honoraria; Daiichi: Honoraria; Parexel: Consultancy; CSL: Consultancy; Sanofi: Consultancy; Quercegen: Research Funding; Incyte: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal